Driving Transformation in Healthcare Payer
BPO UNLEASHING EFFICIENCY.
ENRICHING OUTCOMES.
- End-to-end Revenue Cycle Management Services
- Patient Scheduling and Appointment Management
- Eligibility and Benefits Verification
- Prior Authorization
- Patient Registration / Patient Demographics
- Charge Entry and Charge Audit
- Medical Coding Services
- Clinical Documentation Improvement Services
- Medical Coding Audit and Education Services
- Remittance Processing Services
- Accounts Receivable Services
- Denial Management Services
- Credit Balance Services
- Medical Billing Specialists
- Provider Enrollment and Credentialing Services
Business Process Outsourcing and Technology Solutions for Health Plans

MATURE GLOBAL DELIVERY MODEL | SEASONED HEALTH PLAN BPO PROFESSIONALS | PROPRIETARY AUTOMATION TOOLS
At Access Healthcare, we specialize in providing comprehensive Health Plan BPO services that simplify the clinical and financial experience for patients and healthcare providers. With our intelligent back-office solutions and clinical services, we empower health plans to streamline operations, enhance patient care, and improve outcomes.
Our Healthcare Payer BPO services combine domain expertise, process transformation, and advanced technologies like Conversational AI, RPA, and Analytics to redefine excellence. Leading healthcare organizations trust us to drive innovation, revenue growth, and profitability.
We understand the importance of impacting every healthcare moment along the customer journey, no matter the size or significance. Our tailored solutions leverage next-gen technologies to transform operations. Conversational AI enhances customer interactions, while RPA automates repetitive tasks, improving productivity and accuracy. Analytics provides data-driven insights for informed decision-making. Our approach drives top-line revenues and bottom-line profitability, making us a trusted partner in the healthcare industry.
PARTNER WITH ACCESS HEALTHCARE TO REVOLUTIONIZE YOUR HEALTH PLAN BUSINESS PROCESSES.
Let us reshape your operations, driving innovation, improving patient outcomes, and unlocking growth opportunities. Trust us to be your strategic partner in delivering operational excellence, process improvement, and sustainable success in the ever-evolving healthcare landscape.

BACK OFFICE SERVICES: ADMINISTRATIVE OPERATIONS SUPPORT
- Front End and Digital Mailroom Services
- Claims Operations
- Benefits Configuration Services
- Premium Billing and Collections
- Provider Data Management
- Eligibility and Enrollment Services
- Appeals and Grievances
- Omni-channel Customer Services

FINANCIAL IMPROVEMENT PROCESSES FOR HEALTH PLANS
- Coordination of Benefits/Eligibility Verification
- Overpayment Identification and Recovery and Fraud, Waste, and Abuse Management
- Medicare Star Quality Rating System – Achieving 5-star ratings for Medicare Advantage plans

CARE MANAGEMENT PROCESSES FOR HEALTH PLANS
Utilization Management
Telehealth and Virtual Nursing Services
Integrated Case Management
WHY CHOOSE ACCESS HEALTHCARE?
Intelligent Back Office: Our innovative back-office solutions optimize administrative processes, claims processing, premium billing and collections, configuration services, eligibility, and enrollment services, appeals and grievances, and customer services. We simplify complex processes to ensure efficiency and accuracy.
Payer BPO Financial Improvement Processes: Our expertise in financial improvement processes includes coordination of benefits, eligibility verification, overpayment identification and recovery, fraud, waste, and abuse management, and achieving 5-star ratings for Medicare Advantage plans through the Medicare Star Quality Rating System.
Payer BPO Care Management Processes: We strengthen care management processes through utilization management solutions, telemedicine support, and integrated case management. Our focus is on enhancing patient outcomes and optimizing care delivery.
SUCCESS STORIES
Discover how our Health Plan BPO services have made a tangible impact on the operations and outcomes of health plans like yours. Read success stories from our satisfied clients who have experienced cost reductions, improved efficiency, enhanced patient care, and increased member satisfaction through our tailored solutions.
““I wanted to thank you all again for the hard work and dedication you put into every process you help the Membership Operations team with. The team processed 962 profile update cases during the month of June with a QC score of 100%! Thank you.
“I wanted to reach out after what felt like a successful training meeting with the team today. I was training the team on the end-to-end workflow for Provider Data Cases and as I was going through the SOP, the team made a couple of great suggestions to make the process more efficient. I really appreciated their feedback and want to reiterate how encouraged it is!
READY TO TRANSFORM YOUR HEALTH PLAN OPERATIONS?
Take the first step towards optimizing your health plan operations. Get in touch with our experts today to discuss your specific requirements and explore how our Health Plan BPO services can benefit your organization. Together, we can drive efficiency, improve patient care, and achieve your desired business outcomes.

We understand the importance of efficient scheduling and appointment management in delivering high-quality healthcare services. We aim to streamline the scheduling process, reduce no-shows, and improve patient engagement to ensure the best possible outcomes for providers and patients.
Our Patient Scheduling and Appointment Management services are designed to help healthcare providers manage their schedules more effectively while improving patient satisfaction. Our services include:
Scheduling appointments through the provider’s online portal: We offer a user-friendly online portal that allows patients to schedule appointments at their convenience without waiting on hold or navigating complicated phone systems.
Collecting patient demographics for eligibility and prior authorization requirements: Our team collects all the necessary patient information to ensure eligibility and prior authorization requirements are met before scheduling appointments.
Scheduling appointments based on provider availability: Our scheduling team is designed to match patients with available providers, considering their preferences, availability, and location.
Direct communication with physicians and patients through the messaging system: Our messaging system allows for direct communication between physicians and patients, making it easy to ask questions, share important information, and stay in touch.
Informing patients about their appointments and seeking confirmation: Our system automatically sends appointment reminders to patients and seeks confirmation to minimize no-shows and maximize appointment attendance.
Sending automated reminders to patients and providers: Our system sends automated reminders to patients and providers, reducing the risk of missed appointments.
By leveraging these features, providers can better manage their schedules to minimize long wait times, reduce no-shows, and improve patient engagement. Our Patient Scheduling and Appointment Management services offer several benefits, including:
Reducing no-shows: By sending automated reminders and seeking confirmation, we help reduce the number of no-shows and missed appointments, improving revenue cycle performance.
Improving patient engagement: By providing direct communication with patients and convenient scheduling options, we help improve patient engagement and satisfaction.
Optimizing physician calendars: We match patients with available providers, optimizing physician calendars and minimizing wait times.
Providing a real-time dashboard to physicians showing appointments: We can configure the system to allow physicians to view and manage their schedules easily, ensuring they can provide the best possible care.
Automated reminders and follow-ups: We configure the system to automatically send reminders and follow-ups to patients and providers, ensuring appointments are attended and payments are made on time.
End-to-end tracking of patient payment history and outstanding payments: We track the patient payment history and outstanding payments, making it easy to manage billing and collections.
At Access Healthcare, we understand that scheduling and appointment management are critical components of delivering high-quality healthcare services. Our Patient Scheduling and Appointment Management services are designed to help healthcare providers streamline their operations, reduce no-shows, and improve patient engagement.
Contact us today to learn how your organization can benefit from Wellmed Supply Patient Scheduling and Appointment Management services.

Eligibility and Benefits Verification
At Access Healthcare, we understand that comprehensive eligibility and benefits verification processes are critical for providers to provide prompt, accurate, and thorough information about a patient’s insurance coverage. Our Eligibility and Benefits Verification Services assist healthcare providers in making informed decisions about the nature of care given, medications prescribed, and further diagnostics, particularly in elective and non-emergency procedures, based on the patient’s eligibility.
We believe the absence of proper checks and balances in this process can lead to significant revenue leakages through denials and delayed payments. To avoid this, we provide our clients with insights into the patient’s eligibility upfront before the actual encounter. This information helps healthcare providers suggest a course of treatment aligned with the scope of coverage, classification of out-of-network benefits, and resultant payment obligations.
Our skilled team of experts handles the patient’s eligibility verification process. They have the expertise in confirming the patient’s coverage and benefits from individual payer websites and making phone calls. We assure our clients of a standardized eligibility verification and admission process and guarantee quick turnaround.
ELIGIBILITY AND BENEFITS VERIFICATION SERVICES
Our Eligibility and Benefits Verification Services offer the following benefits to our clients:
Flexible channel for receiving workflows through various patient scheduling systems – EDI, Fax, emails, and FTP files.
Fast and accurate verification of primary and secondary coverage details, including member ID, group ID, coverage period, co-pay, deductible, and co-insurance and benefits information.
Efficient connection with the payer using the best possible channels.
Prompt identification and resolution of missing or invalid data.
Robotic Process Automation for improved speed and accuracy.
Verify patient demographic and policy information, including benefits, deductibles, plan inclusions, and exclusions.
Obtain a pre-certification number and get approval for benefits verification.
Verify the patients’ coverage, co-pays, co-insurance, deductibles, and claims mailing addresses on all primary and secondary payers and update the revenue cycle management system.
Flexible channel for receiving workflows through various patient scheduling systems – EDI, Fax, emails, and FTP files
Fast and accurate verification of primary and secondary coverage details, including member ID, group ID, coverage period, co-pay, deductible, and co-insurance and benefits information
Efficient connection with the payer using the best possible channels
Prompt identification and resolution of missing or invalid data
Robotic Process Automation for improved speed and accuracy.
Verify patient demographic and policy information, including benefits, deductibles, plan inclusions, and exclusions.
Obtain a pre-certification number and get approval for benefits verification.
Verify the patients’ coverage, co-pays, co-insurance, deductibles, and claims mailing addresses on all primary and secondary payers and update the revenue cycle management system.
ACCESS HEALTHCARE’S VALUE PROPOSITION FOR ELIGIBILITY VERIFICATION SERVICES
Our Eligibility Verification Services provide the following benefits to our clients:
Optimal revenue and cash flow.
Reduced patient information-related denials.
Cost savings from global delivery.
Assurance of accurate and complete data.
Fewer rejections for information issues.
Upfront clarification of the patient’s responsibility.
Improved patient satisfaction.
Improved quality.

Prior Authorization
Prior authorization plays a vital role in the healthcare revenue cycle, providing significant protection for both healthcare providers and their patients. It is essential for healthcare providers to adhere to the payer’s guidelines on the facility where the service is rendered, the cost of treatment, the selection of medication, and the coverage status of complex or costly procedures, except in emergency or critical situations. Failure to obtain prior authorization can result in substantial financial liabilities for the patient and revenue loss for the provider.
Healthcare providers are committed to providing the best care possible to every patient who visits their office. One of their primary responsibilities is to select a treatment plan that aligns with the guidelines established by the appropriate payer and educate patients about the optimal options for achieving their desired outcomes. Providers are also obligated to obtain prior authorization from the payer for any anticipated diagnostics, medication, or procedures to ensure that the patient has coverage and access to these services. Physicians may suggest or choose alternative treatment options that fall within the scope of the patient’s coverage to achieve satisfactory outcomes. By providing clarity around these matters, healthcare providers can enhance patient satisfaction and ensure financial protection in line with the payer’s policies.
At Access Healthcare, we specialize in Prior Authorization services to help healthcare providers streamline their revenue cycles and optimize collections. We collaborate with leading solution providers to minimize human effort, enhance quality, and accelerate turnaround times.
PRIOR AUTHORIZATION
Comprehensive analysis of policy/payer details for assessment of coverage
Rapid determination of prior authorization requirements of each patient
Accurate paperwork preparation and timely submissions to the payer
Persistent follow-ups on submitted prior authorization requests
Immediate notification to providers of authorization issues or ambiguities

ACCESS HEALTHCARE’S VALUE PROPOSITION FOR PRIOR AUTHORIZATION SERVICES
Provides clarity on options available under coverage rules
Helps make educated choices of alternatives aligned with coverage
Avoids denials related to coverage issues
Improves patient awareness and satisfaction

Patient Registration / Patient Demographics
Getting complete and accurate information from patients at the point-of-service, and accurately capturing the information in your revenue cycle system is not only essential to the success of your revenue cycle but also enables multivariate population health analytics.
Inaccurate capture of patient demographic information causes claim denials, and consequently, and delayed payments. Research shows that healthcare organizations lose as much as 7% of their annual revenue due to errors in demographic data capture. Establishing a clear and standardized process for collecting patient demographic information helps safeguard against critical mistakes being made at an early juncture. Accurate demographic collection increases the rate of clean claim submissions while reducing payment delays and denials.
Utilize Access Healthcare’s Patient Registration Services to improve accuracy, and optimize your revenue cycle.
DEMOGRAPHIC ENTRY AND VERIFICATION
We validate and update the following patient information on the practice management system:
Legal name, gender, address, phone numbers (work/home/mobile)
Social security numbers for identification
Health insurance information and policy details
Medicaid or Medicare policy
Contact information for the person who is responsible for payments
Special requirements (interpreter, stretcher access, etc.)

WHAT TO EXPECT WITH ACCESS HEALTHCARE’S PATIENT REGISTRATION SERVICES
Rest easy, knowing you have a partner who knows the intricacies of revenue cycle management and business processes and an entire team of process experts on your side. Our team is committed to deeply understanding your organization’s functions from high-level to low-level nuances, and helping you achieve total efficiency.
Our associates are equipped with expertise in all major revenue cycle systems, ensuring:
Improved productivity and accuracy of patient demographic information capture
Increased clean claim submission
Reduced demographic related denials
Real-time collaboration and reporting through our client portals
Detailed status updates and reporting on a weekly basis

Charge Entry and Charge Audit
Failure to effectively document care information can lead to revenue leakage – amounting to millions of dollars of lost revenue. While deploying effective charge capture, workflow solutions can help reduce instances of lost revenue. Also, effective collaboration between coding and charge entry teams leads to a sustainable improvement in the overall process.
With expertise in multiple specialties and Revenue Cycle Platforms, our charge entry experts process a high volume of charge entry transactions with exceptional accuracy. Access Healthcare’s client portal enables smooth communication between our teams, for a seamless end-to-end process.
CHARGE CAPTURE
Our charge entry transactions remain consistent throughout:
Receive documents in the form of superbills, charge tickets, source documents, etc. through FTP or document management system or client’s system.
Capture the date of service, billing provider, referring provider, POS, admission date, CPT/procedure codes, ICD-10, number of units, and modifiers.
Using our proprietary tool ARC.flow, provide real-time reporting to the customer by escalating pending issues for clarification which results in faster turnaround time.
Import charges directly from the EMR. These charges are reviewed for accuracy before being sent for billing.
CHARGE AUDIT
Leverage Access Healthcare’s Charge Audit services to identify missed charges, instances of over-billing, and coding errors that led to revenue loss.
We take an analytical approach to:
Validate written orders for the level of care, and all treatments rendered
Necessary modifiers are appended, and the exact number of units are billed
Comparing charges by patient’s accounts
Verifying charges against updated fee schedule
Identifying undercharges, duplicate posting, and overcharges
Verifying the charges with various department billers and coders
Charge Audits help reveal causes for variances including problems with charge entry, provider absences, failure of providers to report timely charges, a change in coding patterns, services not billed for, and other reasons for claim denials. Ideally, charges should be consistent from month-to-month; barring changes in physician productivity due to unavailability.
Access Healthcare’s Value Proposition for Charge Entry and Charge Audit services
Improve productivity and accuracy
Competency across multiple specialties
Timely filing of claims and benchmarking of fee schedules as well as denial patterns
Review of charge entry processes to mitigate revenue leakage by implementing Charge Audits
Ensure appropriate reimbursement collected
Identify and fix compliance issues for charge overages
Recover lost charges and avoid delay in processing AR
Real-time collaboration and reporting through our client portals

Medical Coding Services
Are you experiencing poor accuracy scores and a slow turnaround time in your medical coding process? The healthcare revenue cycle relies on accurate and quick medical coding. A decrease in these KPIs affects your bottom line. With your team of expert coders from Access Healthcare, you can finally achieve an optimized revenue cycle.
ACCESS HEALTHCARE’S GLOBAL CODING PLATFORM
Coding is a small but essential part of the revenue cycle and often the most daunting. From ICD-10 to changing payer trends, there is much to take your focus away from your primary concern – the patient. Take advantage of Access Healthcare’s Coding and Auditing services to make your revenue cycle run like a well-oiled machine.
Ensure ICD-10 compliance
Reduce AR backlogs
Decrease in DNFB
Improve quality of care
Improve provider documentation
Reduce turnaround times
Enjoy more reliable data reporting
PROCESS. TECHNOLOGY.
Rest easy knowing you have the right people on your team, following a time-tested process, and using top-of-the-line technology. It is like your own coding department without all the expense and hassle.
TRAINING METHODOLOGY AND AUDITS
One of the biggest obstacles to in-house coding is attracting and retaining experienced coders. With Access Healthcare as your partner, you get your team of highly-experienced coders without the inconvenience of lengthy and expensive hiring processes. Each coder deployed to your account is thoroughly vetted, trained, and tested weekly. Audits are built into the process to ensure accuracy at each step.
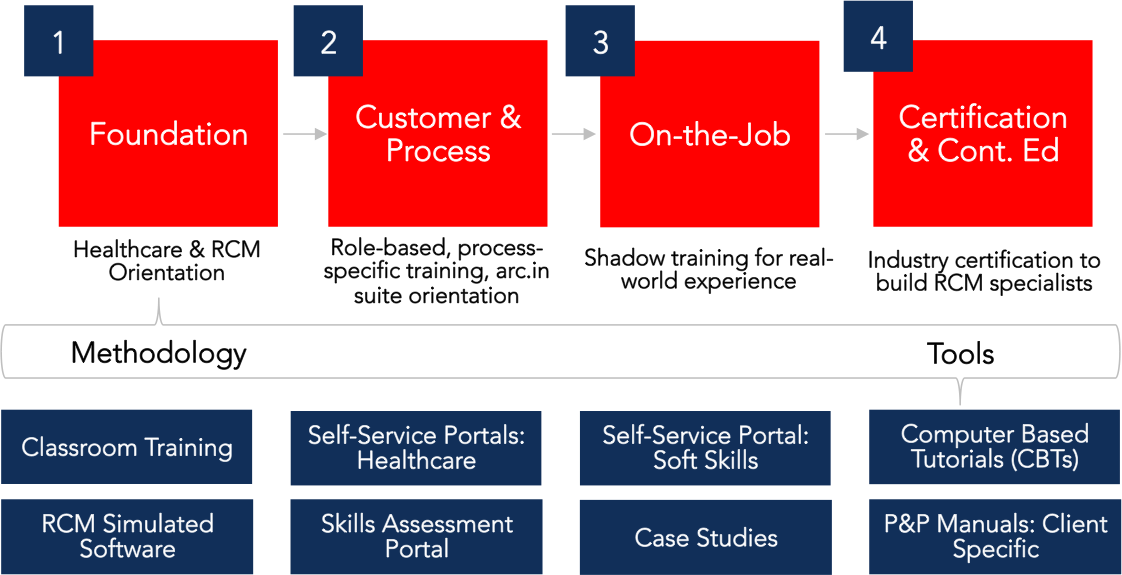
BEST PRACTICES
Transform your revenue cycle management by leveraging Access Healthcare’s simple yet proven process. Understand how coding fits into the larger RCM puzzle with regular updates and suggestions from subject matter experts on ways for continuous improvement.

TECHNOLOGY
Use the arc.in platform to achieve unmatched transparency and oversight to measure productivity and resolve issues. See exactly who is working on your account, what they are working on, and even track their auditing scores. The platform is designed to give you 100% transparency, and peace of mind.

BRING EXCELLENCE TO YOUR BACK-OFFICE REVENUE CYCLE MANAGEMENT
Spend less time worrying about getting paid, and more time on creating great patient experiences. Implement Access Healthcare’s back-office solutions across some, or all your RCM disciplines to unlock value in your revenue cycle.

Clinical Documentation Improvement Services
Your health system’s clinical documentation needs to be clear, consistent, complete, reliable, legible, precise, and timely. Good clinical documentation improves the quality of care, supports better communication, and reduces claim denials…but, achieving all at once may seem impossible when your care team experiences frustration with the documentation process.
Every hospital and health system is different and their needs are unique. Enhance your current CDI program with flexible and built-to-suit CDI services guided by highly skilled and passionate medical professionals. Our competent professionals are experienced in reviewing medical documentation and notifying physicians of inaccurate documentation. Access Healthcare’s clinical documentation integrity services boost performance and ROI along with a variety of other benefits:
Offsite or onsite
Global or domestic
Flexible staffing model
Improved ROI
DRG maximization
Improved ICD-10 code assignment
Increased physician communication
Improved clinical performance
WHY ENHANCE YOUR CDI PROGRAM WITH ACCESS HEALTHCARE?
Making the decision to outsource a portion of your business can be a daunting decision. When that decision affects clinical outcomes and physician processes, it becomes even more nerve-wracking. Ultimately, you must decide what is best for you, your staff, your patients, and the community you serve.
FLEXIBILITY IN STAFFING
Every partnership begins with an onsite component to become familiar with your current clinical documentation practices. And, it opens many cost-effective avenues for you. Whether you wish your CDI program to be fully onsite, offsite, global, domestic, or some combination – you have the flexibility to choose what is right for your organization.
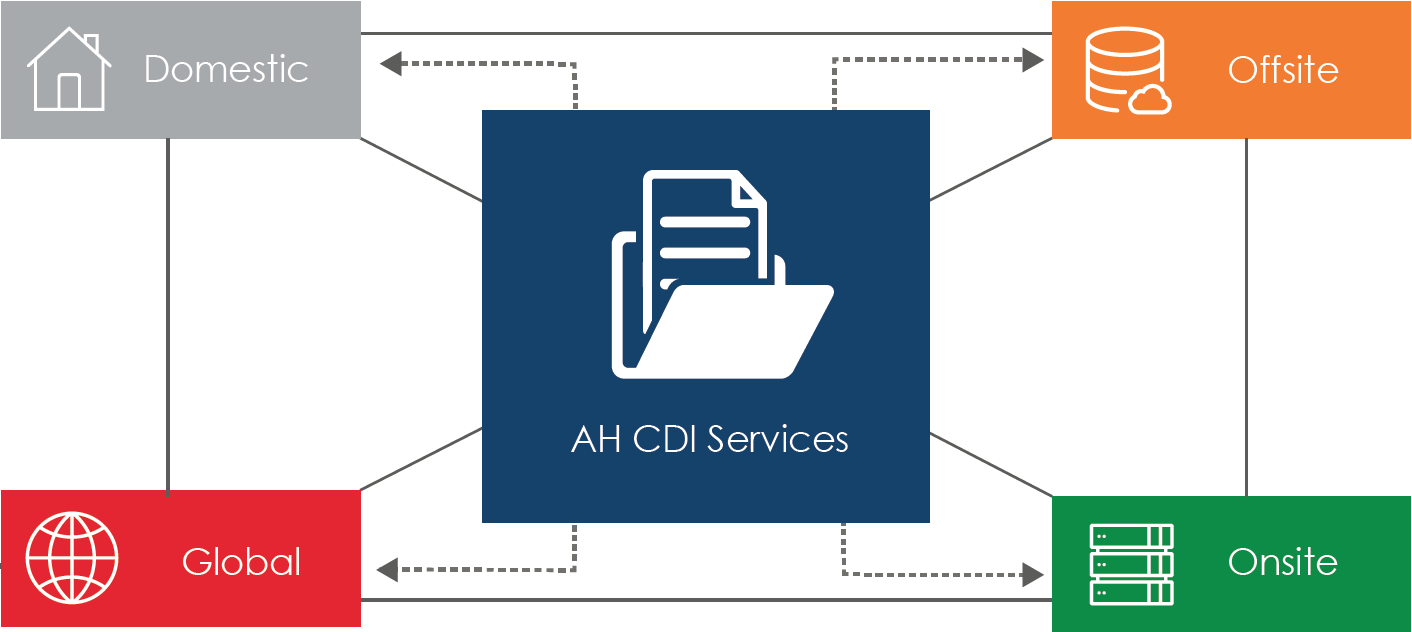
→ Don’t be afraid to go global
Global CDI services are the most cost-effective solution and offer 24/7 support. CDI specialists at Access Healthcare’s global delivery center are highly skilled and undergo extensive training on process, continuous education, and are subject to auditing.
INCREASED COMMUNICATION
One of the trickiest parts of CDI is making sure everyone complies with a set of best practices and takes the necessary time to fully document an encounter. Communication is the key to ensuring all those involved are on the same page and expectations are clearly defined. The right communication pattern for your organization can help keep CDI top of mind and everyone working toward a common goal of improved documentation.

IMPROVE ROI
Improved clinical documentation can affect many things which directly affect ROI. A well-thought-out communication strategy will improve performance and clinical outcomes. Complete and accurate documentation will ensure your organization is paid for the services you provided. Improved documentation will streamline coding efforts, reducing the number of errors or time spent by coders to understand documentation.
CDI VS CODING
A CDI specialist’s job is to ensure the physicians’ documentation is complete and accurate regarding a patient. They can even help the physician determine what DRG the patient has, although it’s ultimately up to the physician. A coder, on the other hand, takes what is documented and assigns a code. Often, a coder can catch errors in documentation, but if a CDI program is in place, this should happen less often.
HOW CDI HELPS YOUR COMMUNITY
Sending quality data to the CDC and other government agencies can improve your chances of receiving grants and funding. In addition, clinical documentation can affect care decisions regarding a patient, both during their current stay and down the road. Making sure that documentation is accurate can improve clinical outcomes.

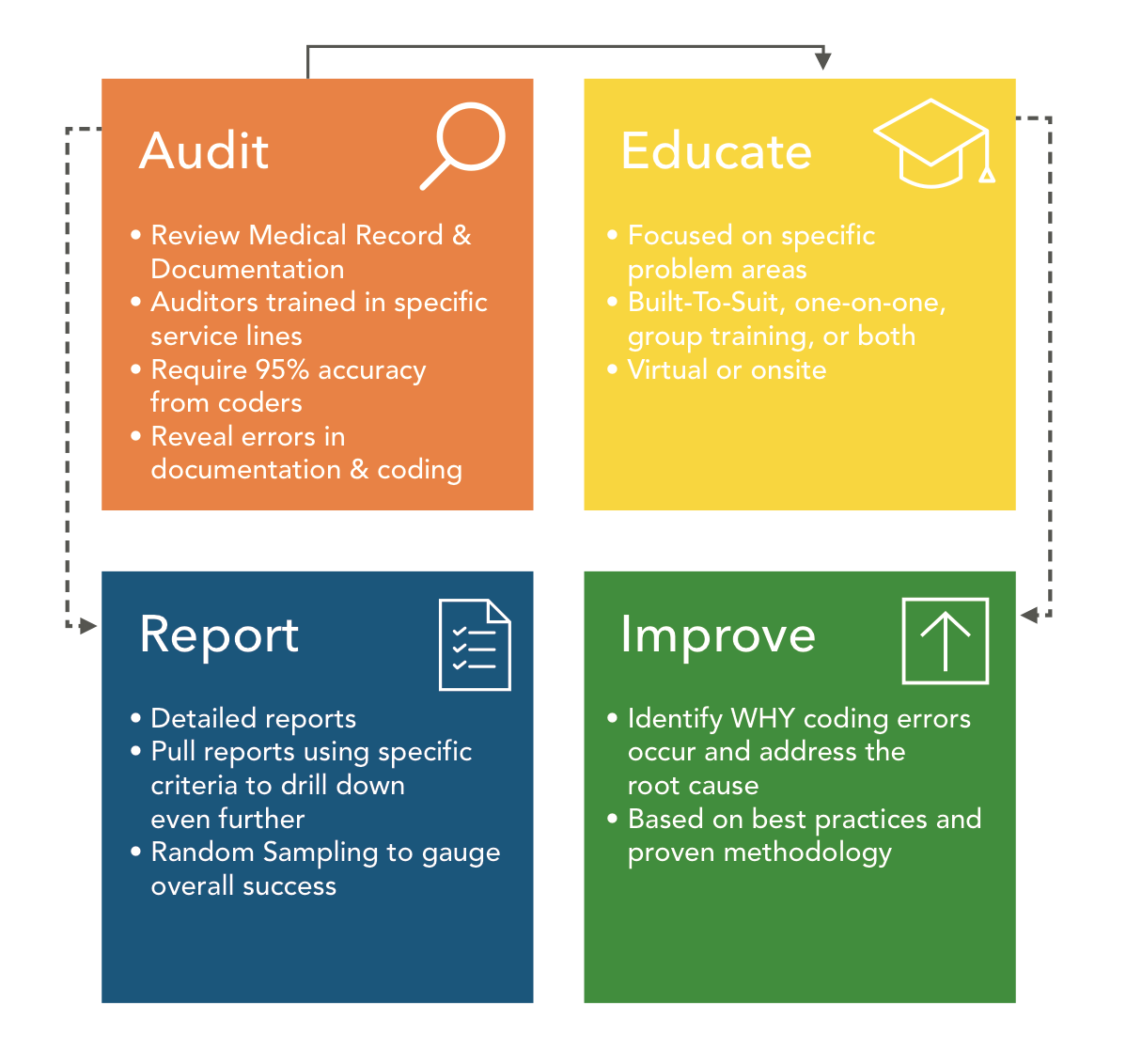
Medical Coding Audit and Education Services
Medical Coding audit and education services from Access Healthcare enable healthcare organisations to arrest revenue leakage by reducing discharges not fully billed, improving coding accuracy, and enabling the coding team to identify physician, facility, or specialty specific coding issues. The findings of our audit team drive clinical documentation improvement initiatives and help the coding team to work with physicians to improve coding accuracy and reduce denials.

Ensure your coding department is operating at peak efficiency and accuracy. Uncover problem areas – from physician documentation, to code compliance, and beyond. Reduce claim denials and get paid accurately for the care you provide.

Take advantage of customizable educational services, built to suit your organization and specific problem areas. Learn from highly trained coding specialists in a group or one-on-one setting.
CODING EXCELLENCE

With ICD-10 and constantly changing government regulations, code auditing and continuing education is more important than ever. Don’t settle for code compliance. Strive for coding excellence. Access Healthcare’s fully customizable code audit and education services can help.
BUILT TO SUIT

Whether you need a one-time audit, ongoing oversight, a complete audit, or a deep dive into one problem area – we help develop a solution that is unique to your organization’s needs. If the result of the audit indicates further education is needed, customize an education program your team members will benefit from most.
PROCESS IMPROVEMENT

Audits are performed by expert coding specialists trained in specific service lines and backed by a company that specializes in end-to-end revenue cycle management. Identify problem areas throughout the revenue cycle that lead to coding inaccuracies, and contribute to revenue loss.
ANALYTICS
Visualize the success of your coding department like never before, with Access Healthcare’s arc.in technology. Pull more detailed reporting, dive into specific areas of interest, and utilize random sampling as a gauge for overall performance.

Remittance Processing Services
While many administrators look at coding and clinical documentation as the key anchors for effective medical billing and consider payment posting to be just the process of posting payments, a good payment processing team can provide critical insights into the overall effectiveness of your revenue cycle processes.
Access Healthcare’s remittance processing professionals don’t just process payments but provide you with trends and reasons for denials, prior-authorization, non-covered services, quality of your clinical documentation and coding processes, and effectiveness of your front-end patient collections.
We process the following types of remittance transactions with an exceptional degree of accuracy and timeliness:
Electronic Remittance Advisory (ERA) Posting. Electronic remittances typically contain a high volume of payment transactions. The processing of ERA batches involves loading the files into the revenue cycle system, processing exceptions from the batch runs by making due corrections using the functionality available on the revenue cycle system.
Manual Payment Posting. Payment information from scanned images of Explanation of Benefit (EOB) documents is captured and each line item is posted to the respective patient accounts. By developing practice and physician-specific business rules along with our team, you will be able to ensure accurate payments, adjustments, write-offs, and balance transfers.
Denial Posting. Our staff is conversant with ANSI denial codes as well as the remark codes used by different payers. We post denials into the customer’s practice management system and take actions such as billing the secondary payer, transferring the balance to the patient account, making adjustments/ write-offs as per defined policies, and routing the denied claims to appropriate work queues.
Posting Patient Payment. Patient payments should be accounted for in order to properly close the claim and avoid any inflated AR. We have extensive experience in processing payments received from patients via different channels like POS cash collections, checks, and credit cards (patient portals). Our payment processing professionals account for patient payments, make decisions on transferring any pending balances to secondary insurers, and resolve any credit balances.

AUTOMATED TOOLS FOR PAYMENT POSTING
Intelligent Payment Processing Platform.
Our intelligent, OCR-enabled payment processing platform, reads printed EoBs in each payment batch and presents all transactions in a tabular format for instant processing of a high volume of payment transactions. The application is also capable of interfacing and synchronizing with any third-party revenue cycle platform.
ACCESS HEALTHCARE’S VALUE PROPOSITION FOR PAYMENT POSTING SERVICES
Analytics. Not only do we provide production and quality report on our performance but also provide inputs on trends in denials, non-covered services, prior authorization, and deductible or co-payment collection issues at the point of service.
Develop Policies for write-off and adjustments. We help our customers develop clearly defined policies for write-offs and adjustments. Based on these policies, we report any unusual contractual adjustments while processing payment transactions.
Handling Denials. We route denied claims to the appropriate coding and denial management team for rework and re-submission to payers in a timely manner.
Filing Claims with Secondary Payers. Identifying claims with secondary payers and processing claims for any remaining balances.
Knowledge Management. Organized business and process rules stored in our knowledge management tool, .Knol helps us keep track of all the updates by providing an effective service.
Dashboards. Dashboards that provide instant access to process health indicators and enable continuous improvement.

Accounts Receivable Services
Reduce your unpaid debt and collect more money at the same time by leveraging time-tested best practices and a proven process to collect payments and reduce backlogs in AR. The result: more money collected faster.

Rest easy knowing your Accounts Receivable (AR) goals are met, and exceeded by a team that understands your organization’s needs. Whether you are a medical billing company, hospital, or healthcare system, we understand the end goal and work tirelessly to achieve it.

Satisfaction is the minimum, but delight is the goal. Improve your revenue cycle process end-to-end, by identifying the reasons for the AR backlogs, not just treating the symptoms. Go above and beyond, and stop the problem before it starts.
AR is an important piece of the revenue cycle. Leverage time-tested best practices, and a proven process to collect payments and reduce AR backlogs. Your result is more money getting collected faster.

BEST PRACTICES
Access Healthcare will analyze your current AR processes to determine areas of improvement through best practices. Benefit from challenging the status quo by continuously targeting and measuring areas for improvement.

A HOLISTIC APPROACH
The revenue cycle can run like a well-oiled machine. The right holistic approach allows for the identification and correction of errors in the revenue cycle that create a backlog of accounts receivables, essentially fixing the problem before it starts.

TECHNOLOGY
Achieve unmatched transparency and oversight to gauge productivity and resolve issues. Our proprietary arc.in workflow management system allows seamless collaboration between teams by providing real-time reports and status updates.


Denial Management Services
Denial Management is one of the most important pieces of a health Revenue Cycle. When insurance companies are denying an average of 9% of claims submitted, in order to ensure a healthy cash flow, healthcare organizations need to focus mainly on root cause and denial prevention.

EVERY MEDICAL PRACTICE EXPERIENCES CLAIM DENIALS.
It’s how those denials are handled that sets exceptional healthcare organizations apart from the rest. However, dealing with claim denials can be a time-consuming task and can take a medical practice’s attention away from what matters most.
Denial management is a critical element to a healthy cash flow, and successful revenue cycle management. Leverage Access Healthcare to quickly and easily determine the cause(s) of denials, mitigate the risk of future denials and get paid faster.
FOCUS ON WHAT MATTERS
Healthcare organizations get paid to make people feel better, and not to run around dealing with insurance companies and tracking down why a claim is denied. Leverage Access Healthcare’s systematic best practices and proven methodology to bring excellence to your revenue cycle management, including the denial management process. Glean insights into why claims are denied, learn how you can avoid denials going forward, and get paid faster.

A SYSTEMATIC, HANDS-ON APPROACH
Each patient is unique when it comes to the care you provide so each denied claim is also unique. Access Healthcare uses a systematic, hands-on approach to ensure each claim receives the attention it needs to be resolved quickly, while also adhering to a strict systematic approach and defined best practices. This ensures maximum results and improved and efficient collections.

ANALYSIS
Each claim is analyzed and researched by an Access Healthcare associate to determine the best course of action.

WORKFLOW
Prioritize claims based on payer, amount, age of bill, or other business rules to ensure maximum benefits.

PREVENTION
Improve the health of your practice and prevent future denials with suggestions for process improvements.
STORY SPOTLIGHT
OBJECTIVE
Find and capture savings
The customer needed to improve overall cash flow and enable easier, more simplified access to revenue. It was imperative to discover the levels of inefficiency through a comprehensive assessment and raise levels of efficiency in other areas burdening financial growth.
SOLUTION
In approximately 30 days, Access Healthcare service experts conducted a comprehensive assessment of the organization’s AR footprint. A summary of the assessment concluded substantial opportunity to improve cash flow in multiple areas totalling $10 million.

Credit Balance Services
Credit Balances can be a liability on your balance sheet and you have more important things to deal with. The last thing you want to think about are accounting errors and refunds. Bring excellence to your Revenue Cycle Management so you can focus on creating great patient experiences.

Billing is the least exciting part of medical care, for both the provider and the patient. Give them one thing less to worry about – knowing you are handling credit balances quickly and looking for ways to avoid them in the future.

Billing is a part of the patient experience. Make every aspect of the care you provide, down to processing refunds, as stress-free and positive as possible by building lasting relationships with patients and insurance companies.
THE RIGHT APPROACH.
Credit balances are no fun. The process of collecting payment is already a major undertaking, and now you must spend additional time and energy trying to give that money back. Leverage Access Healthcare’s Credit Balance Services to quickly and easily resolve these issues.

CUSTOMER SATISFACTION
Professional and timely credit balance handling is essential to keeping a positive relationship with patients, insurance companies, and other payers. Leverage Access Healthcare’s relationships and proven best practices to keep your customers happy.

CONSTANT IMPROVEMENT
Treat the symptoms, and diagnose the cause. The right holistic approach allows for the identification and correction of errors and gaps in the process that lead to credit balance issues, fixing the problem before it starts.

THE RIGHT TECHNOLOGY
Achieve unmatched transparency and oversight to gauge productivity and resolve issues. The arc.in workflow management system allows seamless collaboration between teams by providing real-time reports and status updates.


Medical Billing Specialists
Medical Billing Specialists are an extremely important part of the revenue cycle team in healthcare organizations. Ensure your healthcare organization is operating at peak efficiency. Now you can be connected with the best Medical Billing Specialists in the market, through Access Healthcare.
Access Healthcare’s Billing Specialist model creates an accountability partner to monitor all account activity, identify trends, and conduct deeper research on unresolved AR.
Achieve:
Improved collections
Reduction in unresolved & old AR
Reduction in AR days
Quicker turnaround time
Higher return on investment
Reduced costs
WHAT TO EXPECT…
Knowing you have a partner who understands the nitty-gritty of revenue cycle management gives you confidence that your patients are receiving the best possible experience. Our Billing Specialists act as intermediaries, providing detailed status updates and weekly reports.
Account payments are managed, collected, and posted. Additionally, our team submits claims to payers, and follows up with the insurance companies regularly to ensure the quickest possible turnaround time on payments.
Account information is routinely reviewed to spot trends and opportunities to optimize the revenue cycle processes. Unresolved AR, claim denials, and coding issues are examined for root-cause and forwarded to the client for resolution.
The Billing Specialists’ responsibilities include.
Collecting, posting and managing account payments, submitting claims and following up with insurance companies.
Review account information to identify trends and opportunities to improve the revenue cycle process
Research unresolved and old AR, claim denials, and coding issues (traditionally issues such as these are forwarded to the client to resolve)
Act as client liaison, provide status updates and detailed reporting on a weekly basis

BEST PRACTICES
Leverage Access Healthcare’s best practices engine to bring excellence to your revenue cycle. Your Billing Specialist is highly trained in industry best practices and will oversee each step in the process, continuously targeting and measuring areas for improvement.

Provider Enrollment and Credentialing Services
The process of getting a provider credentialed with a payer involves too many manual steps such as completing application forms, providing clarifications to questions from payers and following up with them to close the credentialing request. With Access Healthcare you can keep your data up-to-date with payers by using our Provider Credentialing Services.
Provider credentialing, the process of getting a physician or a provider affiliated with payers, is a critical step in the revenue cycle. The process enables patients to utilize their insurance cards to pay for medical services consumed and enables the provider to get reimbursed for the medical services provided. Therefore, it is important for healthcare providers to get enrolled and credentialed with maximum payers so that patients can use their insurance plans in your practice – failing to do so will result in the patient looking for competing providers who are enrolled with the health insurance companies they are subscribed to.
However, the process of getting a provider credentialed with a payer involves a lot of manual work in terms of completing the application forms, providing clarifications to questions from payers, and following up with them to close the credentialing request. Trust Access Healthcare to get you credentialed fasters as we understand the forms required by each payer, and their policies and procedures.
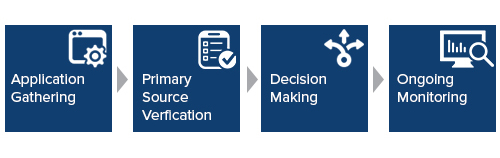
PROVIDER CREDENTIALING
The process involves the following steps:
Application Evaluation. Completing required documentation and identifying exceptions.
Primary Source Documentation. Verify practitioner/ facility information from physicians.
Outbound Call Center. Obtain missing documents and updating the payer’s database.
Follow-up with payers. Follow-up on submitted credentialing requests.
Data Entry. Capture data, label, and link images to specific providers/ facilities in the payer’s database.
Maintenance of Provider Data. Update provider information as per policies and procedures, and CAHQ profile.
PROVIDER ENROLLMENT
Our Provider Enrollment services enable practices to get enrolled for the services they provide by ensuring that payers have the data they need to process claims for the services you provide. We constantly monitor the payers to ensure applications are received and processed on time. We work diligently to identify and resolve potential administrative issues before they impact your provider reimbursements.
The process involves the following steps:
Verification of provider information. Contact payers to determine if they have the correct provider information on file before we submit claims
Updating practice’s Pay-to address. Validate and update the provider’s pay-to address or the billing address
Enrolling for electronic transactions. Our team can enroll providers for four types of electronic transactions:
Electronic Data Interchange (EDI)
Electronic Remittance Advice (ERA)
Electronic Fund Transfer (EFT) and
CSI
Monitoring process. A group of highly skilled team members trained to perform research and analysis on the possible processor functionality gaps.
PROVIDER CREDENTIALING AND ENROLLMENT SERVICES ALLOW YOU TO:
Keep your data up-to-date with payers
Process faster payments from insurance and get more patient referrals
Mitigate revenue leakage
Avoid piles of paperwork and filling out application forms
Reduce denials and identify provider trends
Build relationships with different payers.
Receive real-time status of credentialing and enrollment transactions.
